Where Our Mission Meets Your Calling
Nationwide, there is a growing demand for educated and compassionate palliative care providers. We’re dedicated to meeting that need by providing 12-month post-graduate fellowships for nurse practitioners and physician assistants.
As we follow our mission of Extending the Healing Ministry of Christ, we are committed to growing the clinical, academic and patient experience skills you’ll need to succeed as part of the next generation of APPs at AdventHealth. Our fellowship program is a dedicated year of training and education to prepare you for your role as an advanced practice provider.
Grow Your Skills in Palliative Medicine
Palliative Care is a medical specialty focused on maximizing quality of life through the relief of symptoms during all stages of a serious illness. It is appropriate at any age and can be provided along with curative and life-prolonging treatment. Providers can help treat symptoms like pain, constipation, nausea, dyspnea and anxiety while also assisting in ensuring goals of care for patients and families align with medical treatment.
In our postgraduate fellowship program, you will gain:
- Knowledge in the assessment and management of complex pain-related and non-pain-related symptoms at a sub-specialty level
- A deeper understanding of the complex interaction between serious medical illness and each patient’s goals
- Practice performing spiritual, psychosocial and cultural assessments with referrals to appropriate interdisciplinary members
- Clinical exposure in hospice, oncology and end-stage conditions
- Weekly didactics with program faculty and one-on-one supervision
- Varied rotations at AdventHealth hospitals in the Orlando area
Upon completion of the program, fellows will receive a certificate documenting successful completion and will have the skills and knowledge to successfully pass the Advanced Certified Hospice and Palliative Nurse (ACHPN) examination.
Please note ACHPN certification is only available to nurse practitioners.
About Our Program
Learn about our fellowship program below and see more details in our Program Manual.
- Curriculum
-
Our program goals include:
- Gather, synthesize and apply comprehensive and accurate clinical information from all sources pertaining to the medical care of outpatient/inpatient palliative care patients
- Recognize the presentation, management, disease trajectories and various treatment modalities (chemotherapy, hormonal therapy, immunotherapy, surgery, radiation) for common solid and hematologic malignancies
- Develop competence in pain management for cancer and non-cancer pain for outpatient/inpatient palliative care patients, with a focus on safe opioid prescribing (checking PDMPs, obtaining prior authorizations, documenting prescription refills, fielding other patient requests), monitoring opioid risk scores, screening for substance use disorder and current substance use/misuse, and non-opioid analgesics, adjuvant analgesics and non-pharmacologic approaches
- Develop competency in assessment and management of common non-pain symptoms for palliative care outpatients/inpatients, including, but not limited to:
- Nausea and vomiting (chemo-induced, malignant obstructions, other causes pertinent to cancer)
- Dyspnea
- Insomnia
- Fatigue
- Depression and anxiety
- Existential suffering and grief
- Anorexia/weight loss
- Demonstrate knowledge of alternate routes of administration for medications when patients are unable to take medications orally
- Develop skills in working with an IDT in all aspects of patient care
- Develop skills in communicating/collaborating with oncology providers (hematology/medical oncology, surgical/gynecologic oncology) and other providers (primary care, surgeons, other specialists) while patients are going through cancer treatment
- Demonstrate accurate and comprehensive understanding of psychological stressors and disorders experienced by patients and families facing life-threatening conditions and describe appropriate clinical assessment and management, including the ability to assess, counsel and support patients and families around the burdens of caregiving and make appropriate referrals around fiscal issues and legal concerns
- Curriculum (Continued)
-
Our program goals also include:
- Demonstrate knowledge of local laws and regulations related to the following areas: medical marijuana, physician aid in dying and opioid agonist therapy for opioid use disorder (methadone and buprenorphine)
- Determine relevant scholarly questions and pursue relevant scientific inquiry, particularly regarding topics in outpatient palliative care and supportive oncology
- Effectively communicate across care settings (outpatient, inpatient, hospice) for patients receiving palliative care and demonstrate knowledge of the transitions between these care settings
- Develop competence in discussing end-of-life care in the outpatient/home setting
- Gain experience in related specialties to outpatient palliative care, such as physical medicine and rehabilitation, hematology/medical oncology, gynecologic oncology, radiation oncology and wound care
- Demonstrate care that is respectful of age, developmental stage, gender, sexual orientation and cultural practices
- Maintain a safe and competent practice, including self-evaluation and continuous learning
- Maintain comprehensive, timely and legible medical records
- Demonstrate care that is cost-effective and represents best practices
- Demonstrate the capacity to reflect on personal attitudes, values, strengths, vulnerabilities and experiences to optimize personal wellness and capacity to meet the needs of patients and caregivers
- Fellowship Rotations
-
In our fellowship program, rotations include:
- Inpatient Palliative Care - Core
- Outpatient Palliative Care - Core
- Oncology - Core
- Pulmonary Hypertension - Core
- Intensive Care Unit - Core
- Heart Failure - Core
- Chaplaincy - Core
- Inpatient Hospice - Elective
- Outpatient Hospice - Elective
- Music Therapy/Child Life Therapy - Elective
- Elective of Choice - Inpatient Palliative Care, Outpatient Palliative Care, Oncology, Pulmonary Hypertension, Music Therapy/Child Life Therapy, Heart Failure, Chaplaincy, Intensive Care Unit, Inpatient Hospice, Outpatient Hospice, Research, Leadership/Administrative
- Benefits
-
We want to ensure that it’s rewarding for you to expand your expertise with us. We have made these benefits part of our fellowship program:
- Competitive full-time APP salary
- Professional liability coverage
- Paid leave days
- Medical insurance
- Life insurance
- Disability insurance
- Retirement plan
- Credentialed in our Central Florida Division: 9-hospital system
- Preceptors and Mentorship
-
Every rotation fellow will be assigned a preceptor to help reach their block learning objectives. Palliative Care is supported by an interprofessional team, including Advanced Practice Registered Nurses, Physician Assistants, Physicians, Nurses, Licensed Clinical Social Workers, Chaplains, and other clinical team members. Fellows have mentorship opportunities from any member of the team.
- Completion of Fellowship
-
At the completion of the fellowship, the APPs will be well-prepared to begin their palliative medicine careers and, if applicable, be ready to sit for the ACHPN examination. Fellows will receive an AdventHealth fellowship certification of program completion. Full-time employment offers are contingent upon position availability and performance review.
- Important Dates
-
2026 Fellowship Dates:
Application Opens: N/A Submission Deadline: N/A Interviews and Selection: N/A Notify selected candidates: N/A Credentialing for AHMG: N/A Start Date: N/A End Date: N/A April Cohort Dates: N/A
November Cohort Dates: Coming Soon!
- Interview Process
-
Candidates will be notified if invited for an interview. The interview day will consist of program orientation, committee interview, individual interview and a tour of the AdventHealth Orlando campus.
The interview committee is composed of APPs, physicians and leadership in palliative medicine. The committee will be considering these core competencies:
- Interpersonal communication skills
- Professionalism
- Medical knowledge
- Patient-care experience
- Empathy
- Resilience
- Growth mindset
Candidates are responsible for arranging travel and lodging for the interview day.
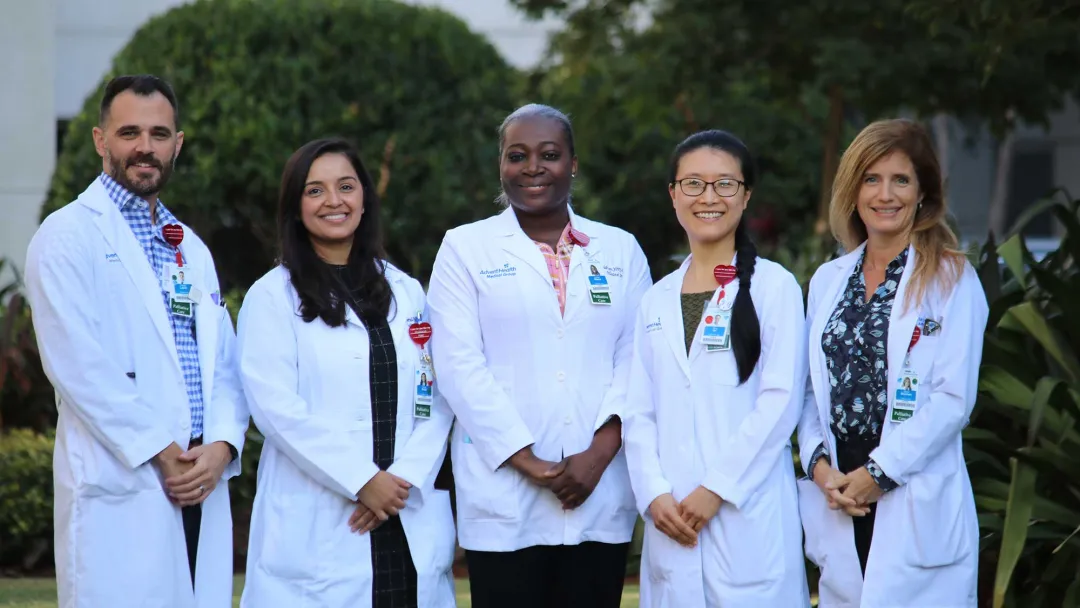
Meet Our Program Team
With a wealth of knowledge and combined decades of experience, our fellowship program team is dedicated to helping you grow your career in palliative medicine.
-

Dana Beller, APRN
Director of APP Fellowship
Lead APP of Palliative Medicine
-

Sandra Pedraza Cardozo, MD
Palliative Care Executive Medical Director
-

Rick Stone, DO
-

Farhana Chowdhury, MD
-

Paige McVey, PA-C
-

Vanessa Ratzlaff, PA-C
-

AnneLouise Aleandre, APRN
-

Nicole D'Amico-Schaal, APRN
-

Linda Pierre, APRN
-

Semira Anbessie, APRN
-
Erin D'Alessandro, APRN
-

Katie Daniel, LCSW
-

Sulan Green, LCSW

Take the Next Step, Apply Today
We welcome your application for our fellowship program in palliative medicine. Our application period for the November 2025 APP fellowship is now closed. We are currently accepting applications for our next cohort to start in November of 2026
Get in Touch With Our Team
To learn more about our fellowship program, please contact:
Dana Beller, APRN, MS, FNP-BC
Director of APP Fellowship, Palliative Medicine APP Fellowship
Dana.Beller@adventhealth.com
Katherine Frazzetta, MMS, PA-C
Assistant Director of APP Fellowship, Palliative Medicine APP Fellowship
Katherine.Frazzetta@adventhealth.com